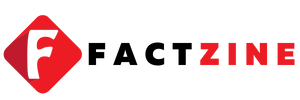
Alcohol and pancreatic cancer are growing public health concerns, with new research suggesting that heavy drinking can dramatically raise the risk for this highly lethal disease and affect people across ages. New findings from a Miami study show that high alcohol intake damages the pancreas’s enzyme-producing cells and triggers inflammation that can set the stage for pre-cancerous changes, with implications for prevention. This inflammatory environment helps form pre-cancerous lesions, reinforcing pancreatic cancer risk factors that scientists are still unpacking as they map how cells respond to chronic exposure and digestive stress. The research also points to Ras mutations pancreatic cancer as a potential collaborator with alcohol-related inflammation in driving disease, suggesting that genetic and environmental factors may work together to transform normal tissue. Experts say that these findings could illuminate new ways to reduce risk through lifestyle changes, more precise screening, and targeted public health strategies that address both behavior and biology.
Viewed through another lens, the link between alcohol use and pancreatic cancer becomes a story about chronic inflammation and cellular change. Excessive drinking can irritate the pancreas, triggering immune responses and molecular pathways that may tilt healthy cells toward abnormal growth. Scientists are exploring how genetic factors and inflammatory signals interact, including the role of growth-control pathways that can be altered in pancreatic tissue. Framing the issue in terms of inflammation, cellular stress, and early tissue changes helps explain why screening and lifestyle adjustments are emphasized in public health messaging.
Alcohol and pancreatic cancer: Understanding the link
Regular drinking could dramatically increase your risk of developing one of the world’s deadliest cancers. Researchers warn that high alcohol intake damages the pancreas’s enzyme-producing cells, triggering inflammation that harms the organ. This inflammatory environment can support the growth of abnormal cells and the formation of pre-cancerous lesions that may evolve into pancreatic cancer. The idea fits within the broader picture of pancreatic cancer risk factors linked to lifestyle and chronic inflammation.
Experts note that heavy drinking is typically defined as eight or more drinks per week for women and 15 or more for men. For progression from inflammation to cancer, a Ras mutation is usually required. This Ras mutations pancreatic cancer step helps explain why not all inflamed pancreata become cancer, and it highlights how genetic factors interact with environmental exposures in this disease.
Heavy drinking pancreatic cancer risk: what the latest research shows
Heavy drinking pancreatic cancer risk is a key focus of recent studies. Scientists in Miami linked long term alcohol use to damage in the pancreas, the organ that controls digestion and blood sugar. The finding underscores how heavy drinking pancreatic cancer risk is shaped by both alcohol induced inflammation and genetic changes such as Ras mutations pancreatic cancer.
These results point to the possibility of preventing cancer by limiting alcohol and by targeting inflammatory pathways. They also remind readers that pancreatic cancer risk factors extend beyond alcohol, requiring a broad approach to prevention and early detection.
CREB gene pancreatic inflammation: the molecular switch driving disease
CREB gene pancreatic inflammation plays a central role in this process. CREB acts as a master controller of inflammatory signals in pancreatic cells, and when activated it can reprogram healthy cells toward abnormal, pre-cancerous states. In laboratory models, CREB drives the sustained inflammation that fuels progression toward cancer.
Crucially, disabling CREB has been shown to stop the formation of pre-cancerous and cancerous lesions in experimental settings. This finding suggests that targeting the CREB gene pancreatic inflammation pathway could form the basis of future pancreatic cancer prevention strategies.
Ras mutations pancreatic cancer: the fatal switch in tumor growth
Ras mutations pancreatic cancer are a key genetic event observed when pancreatic cells move from inflammation to malignant growth. The interaction between alcohol-related inflammation and Ras driven signaling helps explain why most cases of pancreatic cancer carry Ras pathway alterations. Understanding this relationship clarifies why a mutation in the Ras pathway matters for cancer development.
These insights are guiding research toward targeted approaches that interrupt Ras signaling, potentially slowing progression at an early stage and informing how to interpret imaging and biomarker findings alongside lifestyle risk management.
Pancreatic cancer risk factors beyond alcohol
Beyond alcohol use, several factors increase the likelihood of pancreatic cancer. Smoking, being overweight or obese, and the presence of diabetes increase risk, as do red and processed meat consumption and certain blood groups. Age also matters, with higher rates among older adults. Placing alcohol in the broader context of pancreatic cancer risk factors helps people prioritize prevention efforts.
Other contributors include chronic pancreatitis and a family history of the disease. Advances in imaging, such as CT and MRIs, have improved the ability to detect early changes in the pancreas, particularly for those with a strong family or clinical risk profile.
Symptoms and early signs: catching pancreatic cancer early matters
Pancreatic cancer often presents with subtle symptoms at first. Weight loss, fatigue, abdominal pain, and changes in bowel habits are common, and jaundice can appear when the tumor blocks bile flow. Because these signs can resemble less serious conditions, many cases are diagnosed at a late stage, contributing to a poor prognosis.
Recognizing these signs and seeking medical evaluation early improves the chances of catching the disease before it advances. Patients at higher risk due to age, diabetes, or family history should discuss diagnostic options with their clinicians.
Pancreatic cancer prevention strategies: actionable steps
Adopting pancreatic cancer prevention strategies begins with limiting alcohol intake and avoiding heavy drinking. Maintaining a healthy weight, controlling diabetes, not smoking, and eating a balanced diet rich in fiber and vegetables can reduce risk overall and support pancreatic health.
Risk based screening and monitoring, especially for those with a family history or chronic pancreatitis, can help detect precancerous changes sooner. Public health programs and clinician guidance play a role in translating research findings into practical prevention efforts.
Pancreatic cancer biology: the pancreas in health and disease
The pancreas is a 25 cm organ that helps with digestion and hormone regulation. The most common cancer type, pancreatic adenocarcinoma, accounts for about 90 percent of cases and tends to be diagnosed late because symptoms are subtle in early stages.
Chronic inflammation from alcohol or other factors can damage the exocrine tissue and create a pre-cancerous environment. Understanding how CREB and Ras signaling intersect in this tissue helps researchers map the transition from normal function to malignant growth.
Prognosis and survival: what patients should know
Pancreatic cancer carries a grim overall prognosis, with five year survival rates around 10 to 12 percent in the UK and US. The disease is known for its high mortality, and survival declines sharply with advancing stage.
Survival is highly dependent on early detection and tumor biology. While the overall outlook remains challenging, ongoing research into prevention strategies, targeted therapies, and better imaging offers hope for improved outcomes in the future.
Public health perspectives: addressing the silent killer
Pancreatic cancer is often called a silent killer because early symptoms are easy to miss. Public health strategies aim to reduce modifiable risk factors, including heavy drinking pancreatic cancer risk, along with campaigns to promote early screening for high risk groups.
Policies that support smoking cessation, obesity prevention, diabetes management, and better access to advanced imaging can shift the trajectory of this disease. Education about the link between alcohol use and pancreatic cancer helps individuals make informed lifestyle choices.
Diagnostics and imaging advances: CT, MRI, and biomarkers
High tech imaging tools such as CT and MRI have become more sensitive and accessible, allowing earlier detection of pancreas changes and lesions. These advances improve diagnostic confidence and open windows for timely intervention.
Researchers are also exploring biomarkers and functional imaging to complement anatomical scans. Integrating CREB and Ras pathway insights with imaging findings could refine how clinicians assess risk and monitor progression toward pancreatic cancer.
Living with risk: lifestyle choices and resources
For people at risk, small daily choices add up. Reducing alcohol consumption, maintaining a healthy weight, staying physically active, and managing blood sugar can lower overall pancreatic cancer risk and support general health.
Support networks, credible patient education, and access to credible health resources empower individuals to take proactive steps. If you have a family history or clinical risk, discuss monitoring options with a healthcare provider to tailor prevention strategies.
Frequently Asked Questions
How are Alcohol and pancreatic cancer risk connected?
Regular or heavy alcohol use can damage the pancreas and trigger inflammation, increasing the risk of pre-cancerous lesions that may progress to pancreatic cancer. In the studied models, progression often involves Ras mutations, and research also highlights CREB as a pro-inflammatory driver of this process.
What are pancreatic cancer risk factors, and where does alcohol fit in?
Pancreatic cancer risk factors include age, smoking, obesity, diabetes, chronic pancreatitis, and family history. Alcohol consumption is a modifiable factor linked to pancreatic inflammation that can contribute to cancer risk, especially with heavy drinking.
What is the CREB gene pancreatic inflammation link to cancer?
CREB acts as a master regulator of inflammation in the pancreas. Experimental findings show that disabling CREB can stop the development of pre-cancerous and cancerous lesions, highlighting CREB pancreatic inflammation as a potential prevention target.
What role do Ras mutations pancreatic cancer play, especially with alcohol exposure?
Ras mutations drive cell growth and are often necessary for pancreatic cancer progression. Alcohol-related pancreatic inflammation can interact with Ras mutations to promote cancer development in experimental models.
What are heavy drinking pancreatic cancer risk levels?
Heavy drinking is typically defined as eight or more drinks per week for women and 15 or more for men. This level of alcohol intake damages the pancreas, promotes inflammation, and raises the risk of pancreatic cancer.
What are pancreatic cancer prevention strategies related to alcohol?
Key strategies include reducing or avoiding heavy drinking and managing inflammation. The research also points to future prevention approaches that target CREB-driven inflammation, alongside established prevention measures like healthy lifestyle choices.
Can reducing alcohol intake lower the risk of pancreatic cancer?
Yes. Reducing heavy drinking lowers pancreatic inflammation and damage, which can help reduce pancreatic cancer risk. However, risk is multifactorial, and early detection remains important for improving outcomes.
How does knowledge of alcohol-related pancreatic cancer risk help with prevention and detection?
Awareness of alcohol’s role as a pancreatic cancer risk factor supports lifestyle changes, risk assessment, and timely monitoring for early signs. This aligns with pancreatic cancer risk factors and prevention strategies.
| Key Point | Details |
|---|---|
| Study finding | Regular drinking could dramatically increase the risk of pancreatic cancer; the Miami study linked high alcohol consumption to damage of the pancreas’s digestive-enzyme–producing cells, triggering inflammation and the development of pre-cancerous lesions that may progress to cancer. |
| Biological mechanism | Alcohol induces inflammation in the pancreas. A mutation in the Ras gene is typically required for cancer to progress. In experiments, alcohol plus a pro-inflammatory molecule produced pancreatitis-like symptoms, linking inflammation to cancer development. |
| CREB and cancer progression | Researchers found that disabling the CREB gene, which plays a pro-inflammatory role, could stop the formation of pre-cancerous and cancerous lesions. CREB acts like a master controller that can permanently reprogram healthy pancreas cells into abnormal, pre-cancerous cells. |
| Survival and prognosis | Pancreatic cancer generally has a grim prognosis. Five-year survival is about 10–12% in the UK and US, with overall mortality high. Survival varies by stage, but long-term survival remains poor (e.g., around 2% five-year survival in some contexts). |
| Definition of heavy drinking | Heavy alcohol use is defined as eight or more drinks per week for women and 15 or more for men. |
| Rising cases and demographics | There is a troubling rise in pancreatic cancer cases, including among younger people. Improved imaging like CT/MRI may contribute to more diagnoses. Risk increases with age (over 65) and with a history of chronic pancreatitis or family history. |
| Other risk factors | Besides alcohol, risk factors include smoking, being overweight or obese, diabetes, consumption of red/processed meat, and certain blood groups. |
| Symptoms and early detection | Early signs can be subtle: weight loss, fatigue, abdominal pain, changes in bowel habits, and jaundice. Recognizing these symptoms is important for earlier evaluation, though detection is often late. |
| Pancreatic cancer basics | Pancreatic cancer is an umbrella term for tumors of the 25 cm pancreas. The most common type is adenocarcinoma, accounting for about 90% of cases. The organ plays a key role in digestion and hormone regulation. |
Summary
Conclusion: Alcohol and pancreatic cancer is a crucial public health topic. Regular heavy drinking is linked to pancreatic inflammation and the development of pre-cancerous lesions that may progress to pancreatic cancer, underscoring the need for prevention and early detection. Researchers highlight roles for CREB and Ras in cancer progression, suggesting potential avenues for prevention and therapeutic strategies. To reduce risk, awareness of high-risk drinking levels ( eight or more drinks per week for women and 15+ for men ), recognizing early warning signs (weight loss, fatigue, abdominal pain, changes in bowel habits, jaundice), and addressing other risk factors—smoking, obesity, diabetes, and certain dietary choices—are essential. Continued research and public health efforts remain vital to lowering the burden of this deadly disease.